Mutational specificity in liver cancer: why mutant-clones struggle to form tumours
New findings from SPECIFICANCER
Why are certain cancer genes broadly expressed throughout the body, yet they trigger cancer in only specific tissues? New findings from the team taking on our Tissue Specificity challenge suggest that the immune system plays a greater role in this specificity than previously realised.
The key to why certain genes drive cancer in some parts of the body but not others has long been sought but remains elusive. Unlocking this mystery of tissue specificity could enable new preventive strategies and therapies, and might even reveal why some treatments work for people with certain types of cancer but have very little success in others. The Cancer Grand Challenges SPECIFICANCER team is taking on this enduring challenge, guided by the philosophy that a tissue’s pre-existing characteristics dictate whether a mutated gene can drive tumour development.
Major findings recently published by the team in Science have uncovered a new layer of the mystery: the tissue’s interactions with the immune system. Generally, the immune system reacts to abnormal and pre-cancerous cells as if they are pathogens and unleashes a powerful response to eliminate them. However, during tumour development and evolution, cancer cells develop mechanisms to overcome this attack.
Tumours in different tissues escape the immune system through multiple mechanisms. For example, some lung and blood cancers are known to hide from T cells by engaging immune checkpoints. “For other types of cancer, our findings suggest the tumour cells are doing something else – possibly something as yet unknown,” explains SPECIFICANCER team lead Steve Elledge (Brigham and Women’s Hospital, Harvard Medical School).
Immune evasion appears to rely at least partly on tumour-suppressor genes (TSGs), which are normally responsible for restricting tumour growth. When mutated, TSGs can enable abnormal cells to escape the constraints of their controlled environments and become cancerous. Although some TSGs, such as p53, are expressed throughout the body, many TSGs act in a tissue-specific manner. The team’s recent study sheds light on how cancers in different parts of the body develop tissue-specific TSG mutations allowing new mechanisms of immune evasion to be exploited.
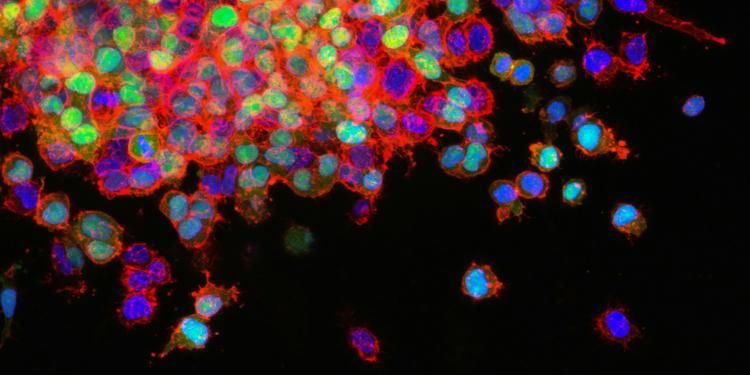
Using the gene-editing tool CRISPR, the team systematically eliminated approximately 7,500 individual genes in two mouse cancer cell lines. To reveal how these genes influence the immune response, the team then implanted the mutated cells into mice with intact immune systems or with severe combined immunodeficiency.
“Our search left us with a huge list of genes which play a role in helping cancer cells hide from the immune system, when mutated,” says Tim Martin, postdoctoral researcher at Harvard Medical School and the lead author of the study. “We were surprised that such a large number of these genes were TSGs. As our study went on, we began to realise there are many more routes for cancer cells to escape the immune system than we thought, and that different tissues do it in different ways.”
The findings provide a new way to think about TSGs and their roles in enabling tumours from different parts of the body to escape the immune system. Furthermore, although the immune system's roles in tumour evolution and the treatment response have been well documented, this study is the first report of the tissue-specific interactions of the immune system with TSGs.
Immunotherapies targeting specific evasion strategies or enhancing the immune response have become a powerful treatment option for some people with cancer. However, most immunotherapies are effective against only certain forms of the disease in only a small proportion of patients. The team’s methods may now provide tools to first understand these variable responses and then develop more effective treatments.
“To learn how to treat cancers in different tissues, we need to understand all the ways they’re escaping the immune system,” says Steve. “Currently, there’s a mismatch between the tools we have in our immunotherapy arsenal and the different mechanisms cancers use to evade attack.” Although TSGs appear to provide many routes for different tumour types to escape the immune system, the team suspects that a finite number of escape strategies exists. “By learning them, we could develop whole new therapeutic approaches to prevent cancer cells from circumventing immune attack,” Steve explains.
Importantly, the study provides a blueprint to explore the evasion strategies of TSGs through analysis of their genetic networks. For example, GNA13 is a TSG that, when mutated, is associated with poor outcomes in certain lymphomas and drives immune evasion in breast cancer. By mutating GNA13 and examining changes in the gene expression network, the team has revealed how mutant GNA13 shields breast cancers from the immune system through secretion of the protein CCL2, which recruits pro-tumour macrophages to the breast microenvironment. Further probing of this mechanism may lead to novel immunotherapies for people with breast cancer.
“This methodical way of exploring how tumours evade the immune system is relatively slow – but it helps to unpack the complexity of these genes in a way we wouldn’t have otherwise,” says Steve. “It’s a new way to consider the challenge of tissue specificity, for sure. We hope others will adopt this approach to work out how other TSGs help tumours evade the immune system and identify new targets for drug development.”
“What’s so exciting about this study is that we ended up following a route we really didn’t expect when we set out,” says Tim. The team began their study by looking for genes that, when perturbed, would boost the immune system’s ability to eliminate cancer cells. “Instead, we found just the opposite.”
Tim recalls the moment when the team realised that their unexpected findings might be meaningful. “We sat chatting in Steve’s office one weekend, and we actually thought the experiment had failed,” he says. “Then from this vast dataset, we realised a lot of genes on our list were TSGs, and that gave us a whole new avenue to explore.”
Steve adds, “There was a gem hiding in what we thought was a failed experiment. Thanks to the flexibility of Cancer Grand Challenges funding, we were able to pursue it.”
The findings were even more fruitful than the team expected. “We thought our investigations might reveal one or two genes for further exploration,” Steve muses. “Instead, we’ve unearthed a new way to think about tissue specificity, and a new way to study the role of TSGs in the immune response – which could ultimately lead to more effective cancer treatments.”
Written by Emily Farthing. The SPECIFICANCER team is funded by Cancer Research UK and the Mark Foundation for Cancer Research.
This article was originally included in our annual progress magazine Discover: A year of scientific creativity.
New findings from SPECIFICANCER
Team SPECIFICANCER: Paving the way for a new era of precision oncology.
New findings from team SPECIFICANCER.